Connect to care 24/7 with Health811
See all the ways we’re connecting you to care.
Find a service
Search for doctors, clinics, mental health services, pharmacies and other health services for you and your family.
Call 811
Talk to a registered nurse — day or night — for free, secure and confidential health advice. Call 811 (
Chat with us online
Send an instant message to a registered nurse, and get answers to health-related questions or concerns.
Talk to your pharmacist
Pharmacists can assess and prescribe medication for common ailments like pink eye, seasonal allergies and skin rashes. They can also extend certain prescriptions for chronic conditions until your next doctors appointment.
Since January 2023, over 4,600 participating pharmacies have conducted over half-a-million assessments for common ailments and issued over 550,000 prescriptions across the province.
Find a long-term care home
Explore your options and apply for long-term care.
Get care at home
Your local home care provider can arrange for nurses and other health care professionals to visit you in your home, and help you access equipment and supplies.
Get reimbursed for health care devices
People with long-term physical disabilities can get help paying for equipment and supplies like wheelchairs and hearing aids.
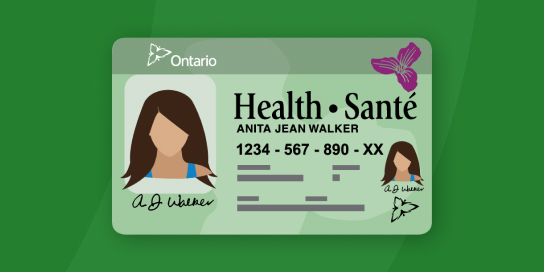
OHIP
OHIP is Ontario’s health care plan. Through OHIP, the province pays for many of the health services you may need.
- Apply for OHIP
- Documents needed to get a health card
- Learn what OHIP covers
- OHIP+
- Renew a health card
- Search for covered drugs
Get temporary health coverage across Canada or outside of Canada.
Get vaccinated
Get a COVID‑19 vaccine or flu shot, and learn about other immunizations.
Health Hiring Hub
Over the next 4 years, we’re investing more than $225 million to expand nursing education in universities and colleges, increasing enrolment by:
- 2,000 registered nurses
- 1,000 registered practical nurses
- 150 nurse practitioners
With these investments, an additional 8,000 nurses will be joining the health care workforce by 2028, boosting our commitment to care whenever and wherever you need it.
Since 2018, hospitals, long term-care homes and other health care institutions have hired:
Over 80,000 nurses
25% were internationally educated
Over 10,000 physicians
38% were internationally educated
Sources:
- Ontario’s Health Professions Database, 2018 to 2022 submissions, and the College of Nurses of Ontario
- Ontario Physician Reporting Centre: Physicians in Ontario, 2018 to 2022 (formerly the Ontario Physician Human Resources Data Centre). Primary data feed is from the College of Physicians and Surgeons of Ontario.
Work or train in Ontario
We are invested in growing our health care workforce, by expanding access to training and reducing financial barriers. Last year alone, we hired 17,000 more nurses registered to work in the province.
If you are an internationally educated nurse, we also offer programs designed to help you become eligible to practice here in only a short time.
Learn about the different careers in health care available to you.
Delivering our Plan for Connected and Convenient Care
We are putting people at the centre of care by making it easier and more convenient for you to access the services you need through:
- providing team-based care to make navigating health care services easier
- delivering care in communities and treating patients in their homes
- making it easier for you to access mental health and addictions services
- reducing wait times for surgeries and performing thousands more surgeries each year
- building 3,000 more hospital beds over 10 years, and adding and upgrading thousands of long-term care beds
$32 billion
For more than 50 health infrastructure projects
$330 million
Ontario’s biggest investment in children’s health care
Learn more about our plan for connected and convenient care.
Learn about more programs and services
Mental health and addictions support
- Find mental health support
- Mental health services for youth
- Know the risks of prescription painkillers
Children and youth
- Free parenting program
- 18-month check-up for babies
- Dental care for children
- Early child development
- Children with special needs
Senior care
- Dental care for low-income seniors
- Exercise and falls prevention programs
- Guide to programs and services for seniors
Cancer care
- Online risk assessment
- Cancer prevention and care
- Prostate cancer screening
- Breast cancer testing and programs
- Cervical cancer testing and prevention
- Colon cancer testing and prevention